What is Glaucoma?
Glaucoma is a group of eye diseases that affects the optic nerve in the eye. The optic nerve takes the visual information from the eye to the brain. Glaucoma damages this nerve and results in vision loss.
When the nerve fibres in the optic nerve are damaged they cannot recover, therefore ay vision lost cannot be recovered.
Therefore it is important that glaucoma is diagnosed early. It needs to be monitored and treated carefully so patients can keep their sight. Indeed the majority of patients, with early diagnosis, regular monitoring and correct treatment maintain useful vision.
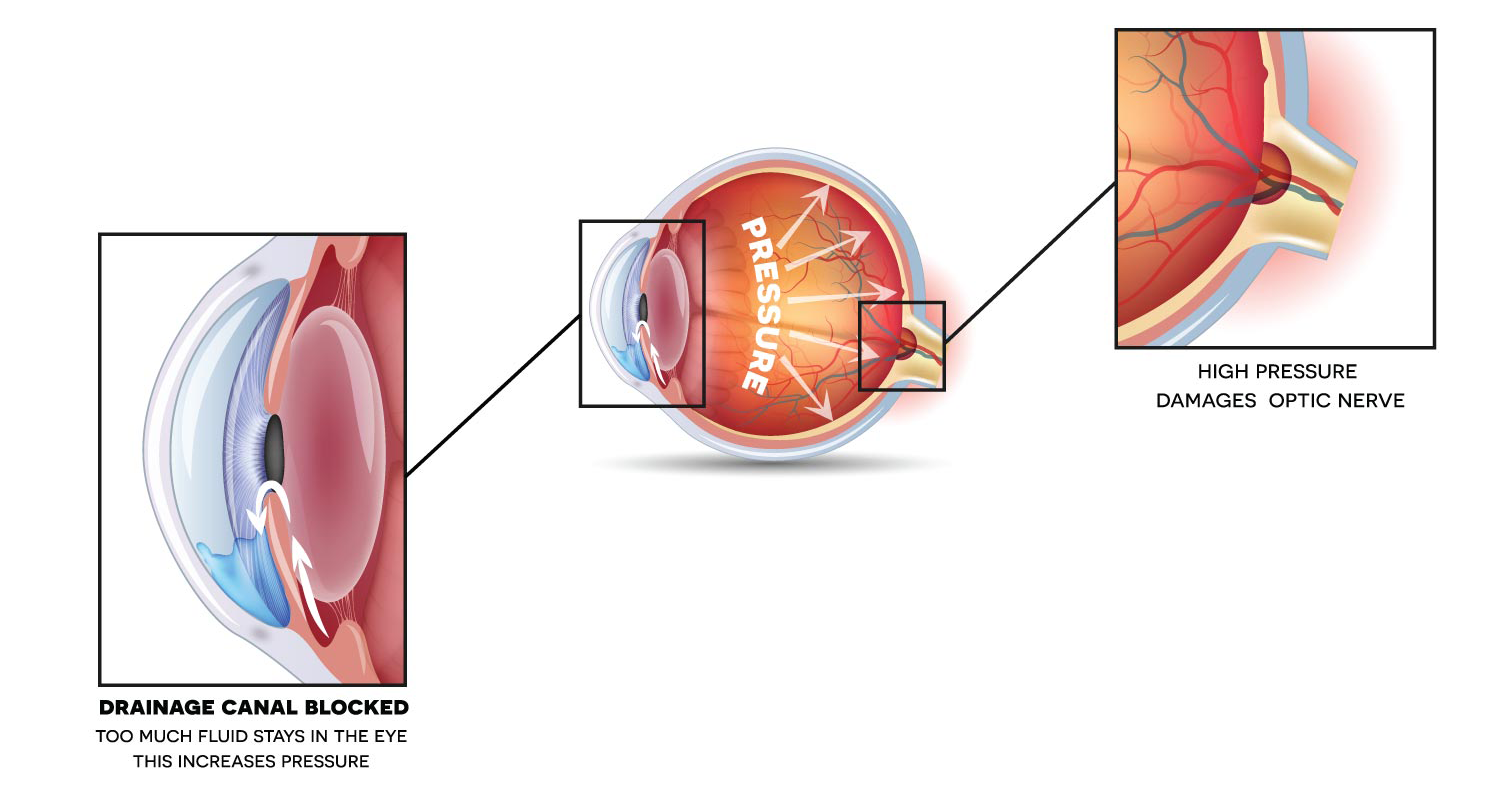
Within the eye, a fluid called aqueous humour flows to allow the eye to function and keep its shape. This results in a pressure within the eye, the intraocular pressure. In glaucoma, the optic nerve damage usually occurs if the intraocular pressure rises to an excessive level that kills the nerve fibres. This leads to sight loss.
However, high pressure does not always cause glaucoma. There are some patients that have damage to their optic nerve due to glaucoma however their eye pressure are the “normal range”. These patients have normal tension (or low tension) glaucoma. Conversely, there are patients whose intraocular pressure is above the “normal range” however they do not have damage to their optic nerve. These patients have ocular hypertension. These patients need to be monitored to see whether they develop glaucoma or be treated to prevent glaucoma developing.
The Eye Structure
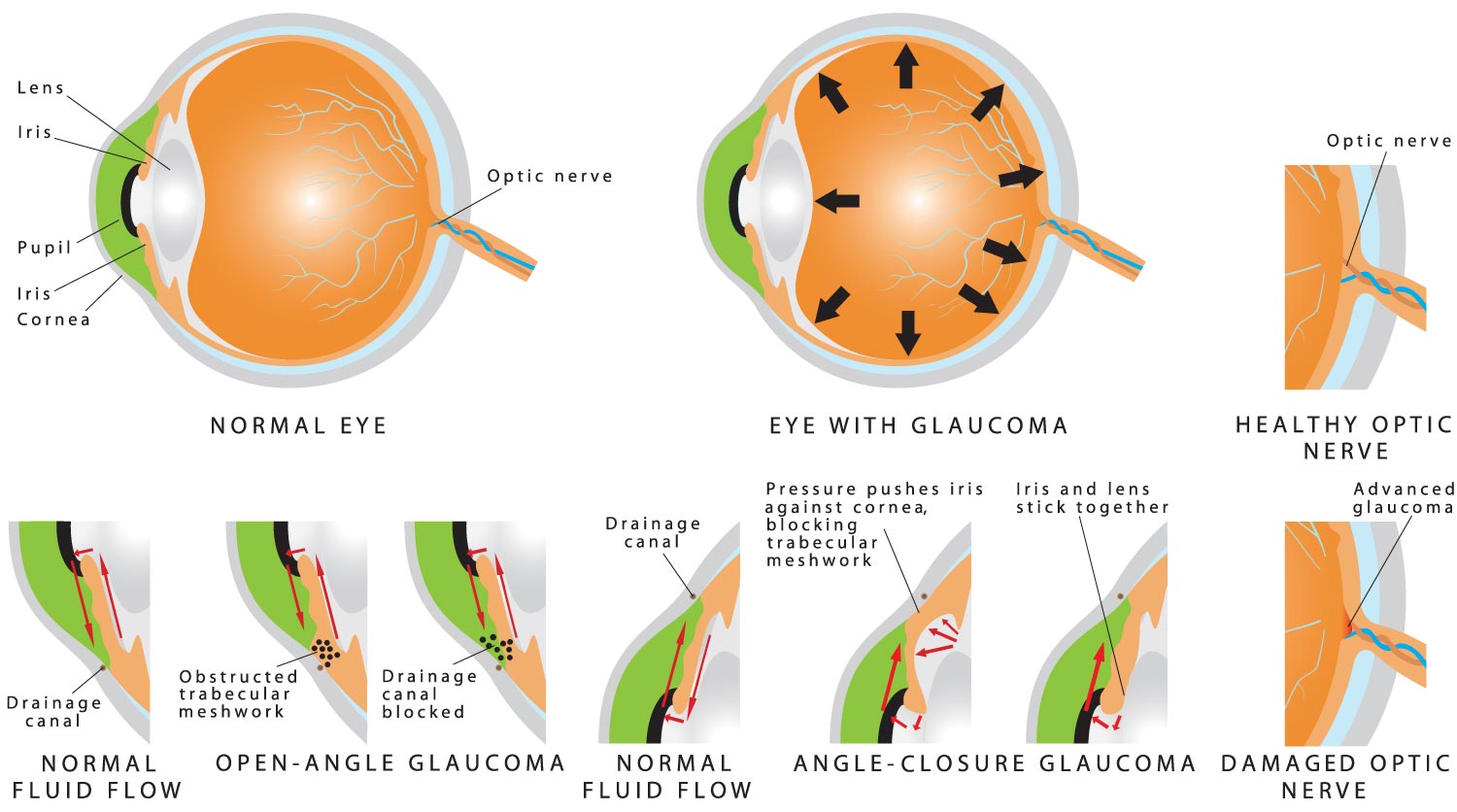
The front of the eye is clear and is called the cornea. The coloured part of the eye is called the iris and is found behind the cornea. The hole within the iris is the pupil and behind this, is the lens of the eye.
Between the iris and the cornea is the drainage angle of the eye, it contains a sieve like structure made up of tiny drainage channels. This is called the trabecular meshwork. Behind the iris is a ring like structure called the ciliary body. Aqueous humour (the fluid within the eye) is made in the ciliary body, flows between the lens and under the iris. It then passes through the pupil and drains out through the drainage angle and trabecular meshwork.
The intraocular pressure is a balance between the production of fluid in the eye and the drainage out of the eye. This balance is upset in glaucoma. Usually in glaucoma, the fluid outflow is restricted resulting in a rise in the eye pressure.
At the back of the eye is the retina, it is on this structure that light is focused by the cornea and lens. The sharpest, most detailed vision is found at the macula, which is found at the central retina. The visual information is sent from the retina and macular to the optic nerve. The optic nerve then takes this information to the brain.
The structure attached under the retina is the choroid, it provides the blood supply to the eye.
Causes of Glaucoma
There is not one single cause of glaucoma. There are risk factors which have cumulative effect. These include a raised intraocular pressure. Others include
Age
The incidence of glaucoma increases with increasing age.
Family History
You are at increased risk of glaucoma if you have a family member with glaucoma. If you have a first degree relative (mother, father, sister, brother or child ) with glaucoma you are at least four times more likely of getting glaucoma.
Ethnicity
Different races are at higher risk of different forms of glaucoma. Afro-Carribeans are at higher the risk of Primary Open Angle Glaucoma. South East Asians are at increased risk of getting Primary Angle Glaucoma.
Short Sightedness (Myopia)
Short sighted or myopic patients are at higher risk of developing glaucoma
Long sighted (Hypermetropia)
Long sighted or hypermetropic patients are at increased risk of developing angle closure
Diabetics
Diabetics may be at higher risk of developing glaucoma
Types of Glaucoma
Primary Open Angle Glaucoma
This is the most common form of Glaucoma in the UK. The drainage angle is open however there is mircoscopic damage to the trabecular meshwork which means the fluid does not properly drain out of the eye. The eye pressure slowly rises in the eye but not to a level that a patient would have any symptoms, however there is damage to optic nerve.
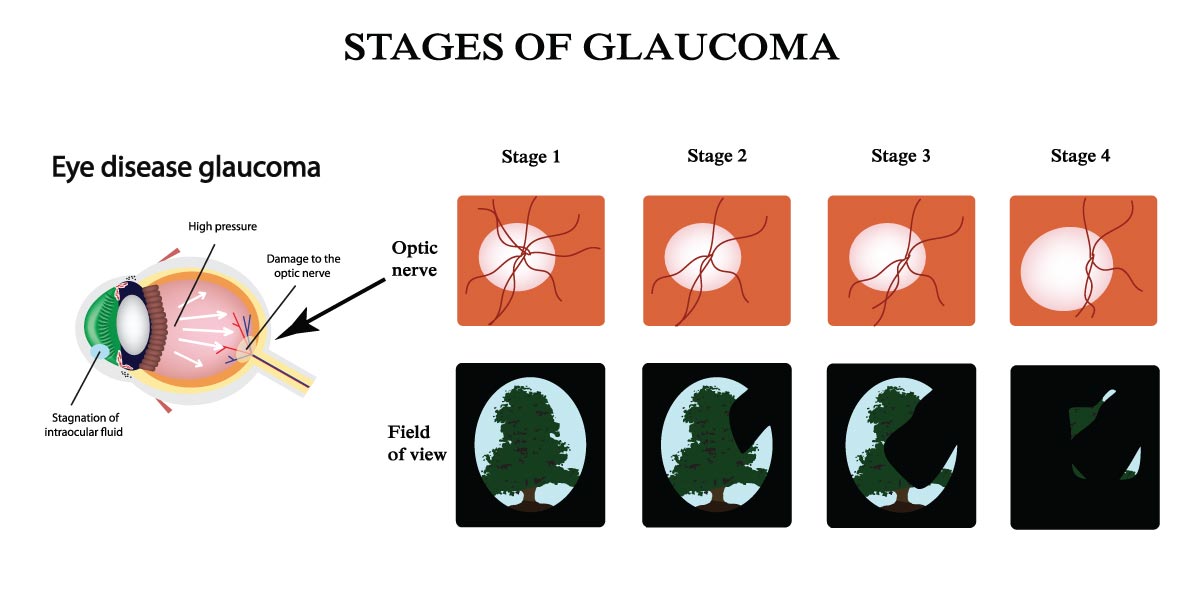
Damage to the optic nerve results in visual field loss. This may not be realised by the patient as the field loss in one eye may be compensated by the other eye, so “filling in” the loss in the visual field. This means that the patient may not realise that there is a problem until there extensive damage.
This is why glaucoma is known as the “silent thief of sight” and the reason why it is important to diagnose and treat glaucoma early.
Primary Angle Closure Glaucoma
In Primary Angle Closure the drainage angle in the eye is occludable, which means aqueous cannot drain through the trabecular meshwork. As the fluid cannot drain the pressure rises in the eye. This can happen very quickly, resulting in a very high intraocular pressure. This usually means the eye becomes painful. It can also become red and/or the vision becomes blurred with halos around bright lights. The pain can be so bad it causes nausea and vomiting. This condition is known as Acute Angle Closure. It can result in permanent vision loss, especially if treatment is delayed. However, if the angle closure attack is treated promptly, the vision recovers.
Sub acute angle closure attacks occur when patients experience mild attacks of raised pressure, resulting in blurring of vision, some pain and redness. This then resolves. If these symptoms happen a patient should be checked. A more chronic or slow developing disease is Primary Angle Closure Glaucoma, where the intraocular pressure rises to level that causes damage to the optic nerve but not at a level that causes symptoms.
The aim of treatment in this condition is to lower the intraocular pressure and open the drainage angle.
Normal Tension Glaucoma (Also know as Low Tension Glaucoma)
In this condition the intraocular pressure is within the normal range (between 10-20mmHg) however there is still damage to the optic nerve. It is thought that poor blood flow to the optic nerve contributes to its damage. Patients wit Raynaunds Syndrome (cold hands/feet) and migraine have a high risk of normal tension glaucoma. This adds to idea that blood flow is important in normal tension glaucoma. If blood pressure is too low it can result in the worsening of the disease. Therefore blood pressure control may be reviewed.
Normal tension glaucoma is treated by lowering the intraocular pressure, usually with pressure lowering drops in the first instance.
Ocular Hypertension
In this condition the intraocular pressure is raised but there is no damage to the optic nerve and no visual field loss. Therefore, there is no detectable glaucomatous damage. However, as these patients have a raised intraocular pressure they are at increased increased of glaucoma. These patients may have to be treated to reduce their risk of developing glaucoma or monitored to start treatment as early as possible if glaucoma does develop
Secondary glaucoma
In these glaucomas there is a cause for the raised intraocular pressure. For example trauma to eye, previous surgery or neovascular glaucoma (in this condition blood vessels grow in the drainage angle of the eye due to conditions like diabetic eye disease). This results in raised pressure. Not only does the glaucoma need to be treated but the original cause may need to be treated.
Congenital Glaucoma
This is a rare condition where there are developmental abnormalities in the eye that result in raised intraocular pressure.
Tests

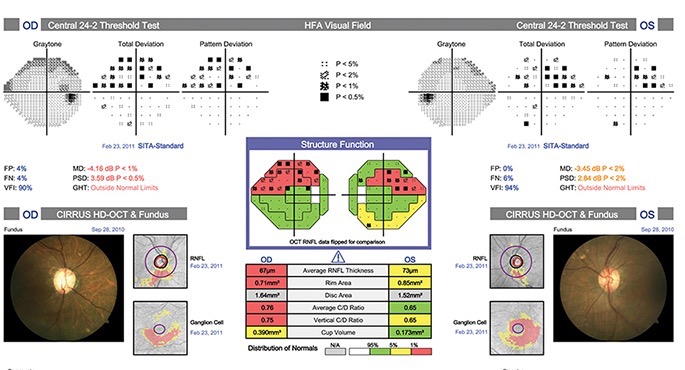
The diagnosis of glaucoma can be difficult and requires several tests. It may not be possible to give a definitive diagnosis at the first consultation.
Tonometry
This is measures the intraocular pressure of the eye. This is carried out by Goldman Application Tonometry not the air puff that a patient may experience at the opticians.
Slit Lamp examination
This allows for examination of the eye especially the optic nerve
Goniscopy
This is the examination of the drainage angle using a special contact lens on the eye
Pachymetry
As the intraocular pressure is not measured directly. It has to be assumed that the cornea is an average corneal thickness. However if a patient’s cornea is thicker than average we are overestimating the pressure and if the cornea is thinner then we are underestimating the pressure. Therefore it is important that the corneal thickness is measured
Visual Field Perimetry
This measures the actual area of sight loss especially in the peripheral vision
Optic nerve imaging
This measures the thickness of the nerve fibre layer of the optic nerve and can detect areas of nerve fibre loss. It can be used to monitor any further loss
Surgical Techniques
Selective Laser Trabeculoplasty (SLT)
Selective laser trabeculoplasty (also called SLT) is a treatment to lower the pressure in the eye/s if you have ocular hypertension or open angle glaucoma. The laser treatment helps fluid to drain from the eye, which in turn lowers the pressure.
Some people respond better to the treatment than others. While the initial treatment may be successful, the pressure can rise again. If this happens the treatment can be repeated, but the results may not be as good as you experienced after the first treatment. Patient’s might need to continue with eye drop treatment as well and, in some cases maybe recommended other treatments including surgery if the pressure is not satisfactory.
Complications are rare but may include inflammation, temporary increase in eye pressure, blurred vision, headache and corneal oedema (clouding of the clear window at the front of the eye).
During treatment patients are normally given drops to make the pupil smaller, which can often cause a slight headache above the eye. Once the patient sits in front of the laser machine further drops are given to numb the surface of the eye.

The doctor will place a special contact lens onto the eye and aim the laser at the part of the eye where the fluid drains (known as the ‘trabecular meshwork’ in the angle between the iris and the cornea). Many patients don’t feel the treatment, but those that do usually describe the pain as mild. It takes about five minutes to treat one eye.
After laser treatment, the eyes will temporarily be dazzled by the treatment but vision should improve in the next few hours. It may help to wear sunglasses to go home.
There is a chance patients get a headache during the first few hours, in which case patients should take their usual painkiller. Patient’s may also need extra drops for a week or so after the treatment and probably be advised to continue with their usual glaucoma drops until their next appointment.
Trabeculectomy
Patient Information
Trabeculectomy
Glaucoma may get worse if the pressure inside the eye is not low enough. Trabeculectomy is recommended when eyedrops are not controlling the pressure and there is a significant risk that glaucoma is going to cause further damage to your sight.
What is a trabeculectomy?
A trabeculectomy is an operation to make the pressure lower inside the eye. It involves making a new channel in the white wall of the eye (sclera), through which fluid flows out into a space underneath the outer layer of the eye (conjunctiva). A successful trabeculectomy creates what we call a ‘bleb’, i.e., a small elevation which is usually covered by the upper eyelid.
Trabeculectomy is usually done as a day case under local anaesthetic. The local anaesthetic is an injection beside the eye, which is given a few minutes before the start of the operation. This makes the eye numb, and usually blurred as well.
What happens during a trabeculectomy operation?
The operation is performed with the patient lying on their back. A paper drape is placed over the face, with fresh air piped beneath it. A clip is used to keep the eye open. You may see light and shadow, but will not see the surgery happening. It usually takes between 40 and 80 minutes to complete the operation, and at the end a patch is taped over the eye, which is left on until the next day.
In many cases, during the surgery, we treat the area of the trabeculectomy with additional medication, to prevent scar tissue from closing the new channel we have created. The medications we use for this include mitomicin-C and 5- fluorouracil (5-FU).
What happens after the operation?
Frequent follow-up is required in the first few weeks after this operation. All patients need to be reviewed the day after surgery then, if all is well, a week later and again one to three weeks after that. The exact timing of these and future reviews depends on how the eye is settling down, and more frequent visits are quite often required.
The first few weeks after the operation are very important for checking the eye and for carrying out adjustments. Most of these adjustments are minor and will be done as part of the outpatient visit. It is best to avoid planning any holiday within two months after the operation.
There will be new drops (an antibiotic and steroid) to use in the eye for several weeks. You won’t need to use your previous glaucoma drops in the eye that has had the operation, although in the longer run some patients do need to restart these to get the pressure low enough. In your other eye, you should continue with any glaucoma drops as before.
What will my vision be like?
It is common for the eye that has had the surgery to be quite blurred for a few weeks, sometimes longer. There is no need to change your glasses straight away, but some patients will benefit from updating their glasses sooner than they normally would, though it’s best to wait for three months while things settle.
You can resume driving (if this applies to you) if your vision is sufficient for you to meet the legal requirements. Trabeculectomy does not improve vision - its purpose is to prevent sight loss in the future.
Returning to work - Most people can return to office based work two weeks after the operation though sometimes longer is needed. It is usually wise to wait at least a month before resuming physically strenuous work or work in a dusty/dirty environment.
Activity - You can use your eyes (for reading, television, computers etc) as soon as you wish - this will not harm your eye. Gentle exercise (walking) is fine, but you should expect to avoid strenuous exercise (running, ball sports, fitness workouts), or lifting heavy objects for at least a month after the operation.
Swimming or immersing the eye should be avoided for at least one month - please ask at your check-up if you wish to resume swimming.
How successful is trabeculectomy?
The operation helps lower the pressure in the eye in about 80% of cases, and most patients will not need glaucoma drops in the eye that has had the operation. A lower pressure is beneficial to nearly all patients with glaucoma, but glaucoma can still progress - in some cases even after a ‘successful’ trabeculectomy.
What are the risks and complications of trabeculectomy?
We always need to consider the risks as well as the potential benefits before going ahead with an operation. The surgeon that has recommended this operation will have judged that the risk to your sight from glaucoma (without the operation) is greater than the risks of the operation itself.
For most patients trabeculectomy achieves a lower pressure without any significant problems; however, all operations do have some risks and for trabeculectomy these include:
- Reduced vision
This is very common in the first two weeks, due to swings in the pressure, minor bleeding inside the eye and inflammation. These typically settle within the first few weeks. Some patients (five to eight percent) may have some degree of permanently reduced vision after the operation. Loss of all vision in the eye due to the surgery itself is very unusual, but as with all intraocular surgery can very rarely occur.
- Discomfort
This usually settles within a few weeks, but some patients experience long-term discomfort. These symptoms are usually mild and can be controlled with artificial tears.
- Increased likelihood of cataract
This is quite common within five years. If it does occur, it can be treated in the normal way. In some patients a trabeculectomy works less well if a cataract operation is performed subsequently.
- Infection and loss of vision in the eye
There is a small risk of infection after any eye surgery including trabeculectomy. Additionally, after trabeculectomy there is a permanently-increased risk of infection getting inside the eye. The risk is small: roughly one in a hundred.
Further surgery may be required to make the operation succeed, or to correct low pressure. It is not unusual for an additional procedure of some sort to be required - usually this is a much shorter procedure than the trabeculectomy itself.
Minimally Invasive Glaucoma Surgery (MIGS)
Micro-invasive glaucoma surgery (MIGS) is the latest advance in surgical treatment for glaucoma, which aims to reduce intraocular pressure by either increasing outflow of aqueous humor or reducing its production. MIGS comprises a group of surgical procedures which share common features. MIGS procedures involve a minimally invasive approach, often with small cuts or micro-incisions through the cornea that causes the least amount of trauma to surrounding scleral and conjunctival tissues. The techniques minimize tissue scarring, allowing for the possibility of traditional glaucoma procedures such as trabeculectomy or glaucoma valve implantation (also known as glaucoma drainage device) to be performed in the future if needed.
MIGS procedures reach their surgical target from an internal route, typically through a self-sealing corneal incision in contrast to traditional surgical techniques using an external technique. By performing the procedure from an internal approach, MIGS procedures often reduce discomfort and lead to more rapid recovery periods While MIGS procedures offer fewer side effects, the procedures tend to result in less intraocular pressure (IOP) lowering than with trabeculectomy or glaucoma tube shunt implantation.
|